AS Level Biology 9700
11. Immunity
Written by: Pranav I
Formatted by: Pranav I
11.1 Defense against disease
External defense system
- Plants make their own organic food via photosynthesis (mostly in leaves)
- Absorb inorganic mineral ions and water from the soil (extensive root systems)
- These materials must be transported to all parts of the plant
Internal defense system (immune system)
- Pathogens successfully enter the body in some cases
- Antigens: A substance that is foreign to the body and stimulates an immune response (proteins, glycoproteins, glycolipids, polysaccharides, toxins and other waste materials)
- White blood cells recognize pathogens by their antigens
- Antibodies: A globular glycoprotein (immunoglobulin; quaternary structure) made by specialised lymphocytes in response to the presence of a specific antigen; each type of antibody molecule has a shape that is complementary to its specific antigen
- Has the ability to distinguish between self and non-self
- Self → refers to substances produced by the body that the immune system does not recognise as foreign (do not stimulate an immune response)
- Non-self → refers to substances or cells that are recognised by the immune system as foreign (stimulate an immune response)
- Immune response: the complex series of responses of the body to the entry of a foreign antigen; it involves the activity of lymphocytes and phagocytes
11.2 Cells of the immune system
- Produced from stem cells in the bone marrow
- Two groups of these cells:
- Phagocytes (neutrophils and macrophages)
- Lymphocytes
Phagocytes
- Produced throughout life
- Stored in the bone marrow before being distributed in the blood
-
Neutrophils form ~60% of the white blood cells
- Travel throughout the body
- Leave blood by squeezing through the walls of capillaries
- Released in large numbers during an infection
- Short-lived cells
-
Macrophages are larger than neutrophils and are found in organs such as the lungs, liver, spleen, kidney and lymph nodes
- Travel in the blood as monocytes
- Develop into macrophages once they leave blood and settle in organs
- Long-lived cells
-
Play a crucial role in initiating immune responses
- Do not destroy pathogens completely
- Cut them up to display antigens that can be recognised by lymphocytes
- Produced throughout life
- Stored in the bone marrow before being distributed in the blood
-
Neutrophils form ~60% of the white blood cells
- Travel throughout the body
- Leave blood by squeezing through the walls of capillaries
- Released in large numbers during an infection
- Short-lived cells
-
Macrophages are larger than neutrophils and are found in organs such as the lungs, liver, spleen, kidney and lymph nodes
- Travel in the blood as monocytes
- Develop into macrophages once they leave blood and settle in organs
- Long-lived cells
-
Play a crucial role in initiating immune responses
- Do not destroy pathogens completely
- Cut them up to display antigens that can be recognised by lymphocytes
Phagocytosis
-
Attraction (chemotaxis)
- Cells under attack by pathogens release chemicals such as histamine
- Pathogens release chemicals
- Passing neutrophils are attracted to the site
-
Recognition and attachment
- Neutrophils have surface receptor proteins that recognise and attach to antibody markers
- Pathogen might also attach directly to the neutrophil membrane
- Endocytosis
- Pathogen trapped within a phagocytic vacuole
- Fusion of lysosomes and phagocytic vacuoles
-
Killing and digestion
- Pathogens digested by enzymes
- Digested products are released by exocytosis
- Neutrophils have a short life → die after digesting some pathogens
- Dead neutrophils collect at a site of infection to form pus
-
Attraction (chemotaxis)
- Cells under attack by pathogens release chemicals such as histamine
- Pathogens release chemicals
- Passing neutrophils are attracted to the site
-
Recognition and attachment
- Neutrophils have surface receptor proteins that recognise and attach to antibody markers
- Pathogen might also attach directly to the neutrophil membrane
- Endocytosis
- Pathogen trapped within a phagocytic vacuole
- Fusion of lysosomes and phagocytic vacuoles
-
Killing and digestion
- Pathogens digested by enzymes
- Digested products are released by exocytosis
- Neutrophils have a short life → die after digesting some pathogens
- Dead neutrophils collect at a site of infection to form pus
Lymphocytes
- Smaller than phagocytes
- Have a large nucleus
- Produced before birth in the bone marrow
-
Two types of lymphocytes:
- B-lymphocytes → remain in the bone marrow until mature and spread throughout the body (concentrate in the liver, lymph nodes and the spleen)
- T-lymphocytes → leave the bone marrow and collect in the thymus (a gland in the chest) for maturation
- Only mature lymphocytes can carry out immune responses
- Different types develop during maturation → each specialised to respond to one antigen
- Circulate between the blood and the lymph → distributed throughout the body, and come into contact with pathogens & each other
- Immune response depends on B and T cells interacting with each other
B-lymphocytes
- Gains the ability to make just one type of antibody as it matures (genes are changed)
- Each B cell then divides to make a small number of identical cells (clone)
-
Each B cell uses part of the antibody molecule to make receptors in the CSM
- Can combine with one specific antigen
- To recognise antigens when they enter the body
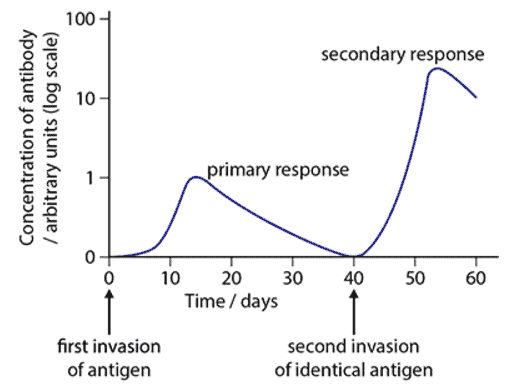
- Primary immune response: the first immune response to a specific antigen
- Clonal selection: during an immune response the only lymphocytes to respond are those with receptors specific to antigens on the surface of the invading pathogen
- Clonal expansion: the increase in number of specific clones of lymphocytes by mitosis during an immune response
- Plasma cells: Short-lived, activated B-lymphocytes produced during clonal expansion; produce and release antibody molecules into the blood, lymph or onto the linings of the lungs and the gut
- Antibodies stay in the blood for longer than the plasma cells
-
Memory cells: Long-lived, activated B-lymphocytes that are specific to one antigen; activated to differentiate into plasma cells during secondary immune responses to the specific antigen
- Divide rapidly and develop into plasma cells and more memory cells during secondary immune responses
- Faster response due to the presence of many memory cells of the specific clone
- Basis of immunological memory (the ability of the immune system to mount a larger and more rapid response to an antigen that has already been encountered before)
- More antibodies are produced in the secondary immune response due to the presence of many more B cells specific to the antigen (size of clone increases during the primary immune response)
B cells and antibodies
-
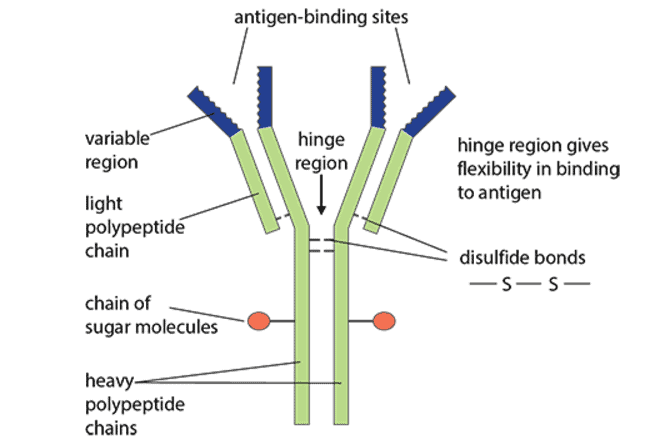
Each antibody molecules has four polypeptide chains: two ‘long’ or ‘heavy’ chains and two ‘short’ or ‘light’ chains
- Disulfide bonds hold the chains together
- Each antibody molecule has two identical variable regions (has parts of both light and heavy chains)
- Each clone of B cells makes antibodies with the same variable regions → complementary in shape to one antigen
- ‘Hinge’ region gives the flexibility for the antibody to bind to antigens on the surface of a pathogen
- IgG → two antigen-binding sites (four polypeptide chains) ; IgA → four antigen-binding sites ; IgM → ten antigen-binding sites
-
Ways in which antibodies work to protect the body from pathogens
- Combine with viruses, preventing them from entering or damaging cells
- Attach to flagella of bacteria, making them less active and easier for phagocytes to engulf
- Cause agglutination of bacteria, reducing the chances of spread throughout the body (if they have multiple antigen binding sites)
- Perforate the cell walls of bacteria, causing them to burst when they absorb water by osmosis
- Coat bacteria, making it easier for phagocytes to ingest them; phagocytes have receptor proteins for the constant regions of antibodies
- Antitoxins combine with toxins, neutralising them and making them harmless
T-lymphocytes
- Specific cell surface receptors → T-cell receptors
- Each are specific to one antigen
- Activated when they recognise this antigen on another host cell
-
Antigen presentation: the process of preparing antigens and exposing them on the surface of host cells for recognition by T-lymphocytes
- Macrophages that have engulfed a pathogen
- Body cells that have been invaded by a pathogen
- Clonal expansion of T cells occurs
-
Types of T cells
-
T-helper cells → secretes cytokines (any signalling molecule released by cells to influence the growth and/or differentiation of cells) to coordinate activity during immune responses
- Release cytokines
- Stimulate appropriate B cells to divide into plasma cells (secrete antibodies) and memory cells
- Some also stimulate macrophages to carry out phagocytosis more vigorously
- Some also stimulate T-killer cells to divide by mitosis and to differentiate by producing vacuoles full of toxins
-
T-killer (T-cytotoxic) cells → Attaches to cells, releases toxic substances to kill infected cells and cancer cells
- Search for antigen presenting body cells with their specific antigen
- Punch holes in CSM of infected body cells
- Secrete toxic substances (e.g. H2O2)
- Kill the body cells and pathogens inside
- Memory T-helper cells and memory T-killer cells are produced → remain in the body and become active during secondary immune responses
- Specific cell surface receptors → T-cell receptors
- Each are specific to one antigen
- Activated when they recognise this antigen on another host cell
-
Antigen presentation: the process of preparing antigens and exposing them on the surface of host cells for recognition by T-lymphocytes
- Macrophages that have engulfed a pathogen
- Body cells that have been invaded by a pathogen
- Clonal expansion of T cells occurs
-
Types of T cells
-
T-helper cells → secretes cytokines (any signalling molecule released by cells to influence the growth and/or differentiation of cells) to coordinate activity during immune responses
- Release cytokines
- Stimulate appropriate B cells to divide into plasma cells (secrete antibodies) and memory cells
- Some also stimulate macrophages to carry out phagocytosis more vigorously
- Some also stimulate T-killer cells to divide by mitosis and to differentiate by producing vacuoles full of toxins
-
T-killer (T-cytotoxic) cells → Attaches to cells, releases toxic substances to kill infected cells and cancer cells
- Search for antigen presenting body cells with their specific antigen
- Punch holes in CSM of infected body cells
- Secrete toxic substances (e.g. H2O2)
- Kill the body cells and pathogens inside
-
T-helper cells → secretes cytokines (any signalling molecule released by cells to influence the growth and/or differentiation of cells) to coordinate activity during immune responses
- Memory T-helper cells and memory T-killer cells are produced → remain in the body and become active during secondary immune responses
11.3 Active and passive immunity
-
Active immunity: immunity gained when an antigen enters the body, an immune response occurs and antibodies are produced by plasma cells
- Natural active immunity → gained by being infected by a pathogen
- Artificial active immunity (vaccination) → gained by putting antigens into the body, either by injection or by mouth
- Provides permanent (long-term) immunity
- Takes time for enough B and T cells to be produced
-
Passive immunity: the temporary immunity gained without there being an immune response
- Natural passive immunity → gained by a fetus when maternal antibodies cross the placenta, or when an infant consumes breast milk (+ colostrum - contains IgA antibodies)
- Artificial passive immunity (e.g. antitoxins) → gained by injecting antibodies
- Person does not produced the antibodies themselves
- B and T cells have not been activated
- Provides temporary (short-term) immunity
-
Active immunity: immunity gained when an antigen enters the body, an immune response occurs and antibodies are produced by plasma cells
- Natural active immunity → gained by being infected by a pathogen
- Artificial active immunity (vaccination) → gained by putting antigens into the body, either by injection or by mouth
- Provides permanent (long-term) immunity
- Takes time for enough B and T cells to be produced
-
Passive immunity: the temporary immunity gained without there being an immune response
- Natural passive immunity → gained by a fetus when maternal antibodies cross the placenta, or when an infant consumes breast milk (+ colostrum - contains IgA antibodies)
- Artificial passive immunity (e.g. antitoxins) → gained by injecting antibodies
- Person does not produced the antibodies themselves
- B and T cells have not been activated
- Provides temporary (short-term) immunity
Vaccines
-
A preparation containing antigens which is used to stimulate an immune response artificially
- Whole live microorganism
- Dead microorganism
- Attenuated microorganism
- Toxoid (harmless form of toxin)
- Surface antigens
- Given by injection into vein/muscle OR taken orally
-
Vaccines that do not mimic an infection (lacking live microorganisms) are less effective
- Need booster injections to stimulate secondary responses
-
Herd immunity: vaccinating a large proportion of the population; provides protection for those not immunised as transmission of a pathogen is reduced
- Interrupts the transmission cycle
- 93-95% required to prevent transmission in a population
-
A preparation containing antigens which is used to stimulate an immune response artificially
- Whole live microorganism
- Dead microorganism
- Attenuated microorganism
- Toxoid (harmless form of toxin)
- Surface antigens
- Given by injection into vein/muscle OR taken orally
-
Vaccines that do not mimic an infection (lacking live microorganisms) are less effective
- Need booster injections to stimulate secondary responses
-
Herd immunity: vaccinating a large proportion of the population; provides protection for those not immunised as transmission of a pathogen is reduced
- Interrupts the transmission cycle
- 93-95% required to prevent transmission in a population
Vaccination programmes
- Schedule of vaccinations adopted by countries across the world to their own circumstances
- Large population of children in the target age group are vaccinated → herd immunity achieved
- Also protects against new diseases transmitted by visitors, migrants or returning travellers
- Used to contain outbreaks of disease → ring immunity: vaccinating all those people in contact with a person infected with a specific disease to prevent transmission in the immediate area
- One-dose vaccinations fail to eliminate diseases despite high coverage → poor response to the vaccine shown by some children (need at least 1 booster to develop full immunity)
- Schedule of vaccinations adopted by countries across the world to their own circumstances
- Large population of children in the target age group are vaccinated → herd immunity achieved
- Also protects against new diseases transmitted by visitors, migrants or returning travellers
- Used to contain outbreaks of disease → ring immunity: vaccinating all those people in contact with a person infected with a specific disease to prevent transmission in the immediate area
- One-dose vaccinations fail to eliminate diseases despite high coverage → poor response to the vaccine shown by some children (need at least 1 booster to develop full immunity)
Monoclonal antibodies
-
Monoclonal antibodies (Mabs): antibodies made by a single clone of hybridoma cells; all the antibody molecules made by the clone have identical variable regions so are specific to one antigen
- B cells that divide by mitosis do not secrete antibodies
- Plasma cells that secrete antibodies do not divide
- Specificity of antibodies has made them useful in the diagnosis and treatment of diseases
- Hybridoma: a cell formed by the fusion of a plasma cell and a cancer cell; it can both secrete antibodies and divide by mitosis
-
Monoclonal antibodies (Mabs): antibodies made by a single clone of hybridoma cells; all the antibody molecules made by the clone have identical variable regions so are specific to one antigen
- B cells that divide by mitosis do not secrete antibodies
- Plasma cells that secrete antibodies do not divide
- Specificity of antibodies has made them useful in the diagnosis and treatment of diseases
- Hybridoma: a cell formed by the fusion of a plasma cell and a cancer cell; it can both secrete antibodies and divide by mitosis
Using monoclonal antibodies in diagnosis
- Used to locate the position of blood clots caused by deep vein thrombosis
- Mouse injected with human fibrin
- Makes plasma cells that secrete antibodies against fibrin
- Collected from the spleen of the mouse
- Plasma cells fused with cancer cells to form hybridomas (secrete antifibrin antibodies)
- Radioactive chemical that produces gamma radiation is attached to each antibody molecule to make radioactively labelled Mabs
- Introduced into the patient’s blood
- Bind to fibrin molecules present in blood clots
- Radioactivity emitted by these labelled antibodies is used to detect their location (gamma-ray cameras are used)
- Routinely used in blood typing and tissue typing
- Used to locate the position of blood clots caused by deep vein thrombosis
- Mouse injected with human fibrin
- Makes plasma cells that secrete antibodies against fibrin
- Collected from the spleen of the mouse
- Plasma cells fused with cancer cells to form hybridomas (secrete antifibrin antibodies)
- Radioactive chemical that produces gamma radiation is attached to each antibody molecule to make radioactively labelled Mabs
- Introduced into the patient’s blood
- Bind to fibrin molecules present in blood clots
- Radioactivity emitted by these labelled antibodies is used to detect their location (gamma-ray cameras are used)
- Routinely used in blood typing and tissue typing
Using monoclonal antibodies in treatment
- Need to be administered more than once
- Antibodies are produced by laboratory animals → trigger an immune response because they are non-self and acts as antigens
-
Humanising Mabs in two ways:
- Altering the genes that code for the heavy and light polypeptide chains of the antibodies so that they code for human sequences of amino acids
- Changing the type and position of the sugar groups that are attached to the heavy chains to the arrangement found in human antibodies
- Need to be administered more than once
- Antibodies are produced by laboratory animals → trigger an immune response because they are non-self and acts as antigens
-
Humanising Mabs in two ways:
- Altering the genes that code for the heavy and light polypeptide chains of the antibodies so that they code for human sequences of amino acids
- Changing the type and position of the sugar groups that are attached to the heavy chains to the arrangement found in human antibodies