AS Level Biology 9700
8. Transport in mammals
Written by: Rhia Sakthivel
Formatted by: Pranav I
Index
8.1 The circulatory system
- The circulatory system in mammals is a closed system, meaning blood stays within the vessels as it circulates
- Blood completes a double circulation, passing through the heart twice in one full circuit
- Systemic circulation
- Blood is pumped from the left ventricle into the aorta, delivering oxygen and nutrients to the body
- Deoxygenated blood returns to the right atrium through the vena cava
- Pulmonary circulation
- From the right ventricle, blood is pumped to the lungs via the pulmonary arteries, where gas exchange occurs
- Oxygenated blood returns to the left atrium through the pulmonary veins
- The systemic circulation operates at a higher pressure than the pulmonary circulation, ensuring efficient delivery of oxygen and nutrients
- The human circulatory system is closed double circulation
8.2 Blood vessels
- The circulatory system is composed of three main types of vessels: arteries, veins, and capillaries
- Arteries carry blood away from the heart
- Veins carry blood towards the heart
- Small arteries are called arterioles, and small veins are called venules
- Capillaries connect arterioles and venules, bringing blood close to nearly every cell in the body
Arteries and arterioles
- Arteries transport blood swiftly and at high pressure to tissues, away from the heart
- Artery walls are strong and elastic, able to withstand high pressures like 120 mmHg (16 kPa) in the aorta
- Artery and vein walls consist of three layers:
- Inner layer: endothelium with flat squamous epithelium and elastic fibres (smooth to reduce friction)
- Middle layer: smooth muscle, collagen, and elastic fibres
- Outer layer: elastic and collagen fibres
- Arteries have the thickest walls among blood vessels
- The aorta has a 2.5 cm diameter and 2 mm wall thickness near the heart
- Elastic arteries (e.g. aorta) have many elastic fibres in their middle layer to stretch and recoil, preventing bursts and evening out blood flow
- Muscular arteries, with more muscle and less elastic tissue, transport blood closer to its destination and regulate flow through smooth muscle contraction
- Arterioles, derived from muscular arteries, slow blood flow for effective gas and nutrient exchange in capillaries. They respond to nerve impulses and hormones, causing:
- Vasoconstriction → narrowing and redirecting blood low
- Vasodilation → increasing blood flow

Capillaries
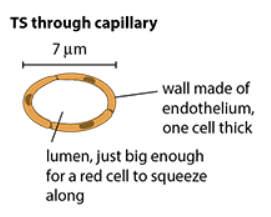
- Arterioles branch into capillaries (the smallest blood vessels) forming networks called capillary beds throughout most tissues (except the brain, cornea, and cartilage)
- Capillaries function is to bring blood close to cells, enabling rapid exchange of substances between blood and cells
- Capillaries are around 7 μm in diameter, similar to the size of red blood cells, allowing cells to squeeze through and be within 1 μm of surrounding cells needing oxygen
- Capillary walls are extremely thin, consisting of a single layer of endothelial cells with tiny gaps that enable components of blood to seep into surrounding tissues
- Blood pressure decreases significantly in capillaries, dropping from about 35 mmHg (4.7 kPa) at entry to about 10 mmHg (1.3 kPa) at the exit end
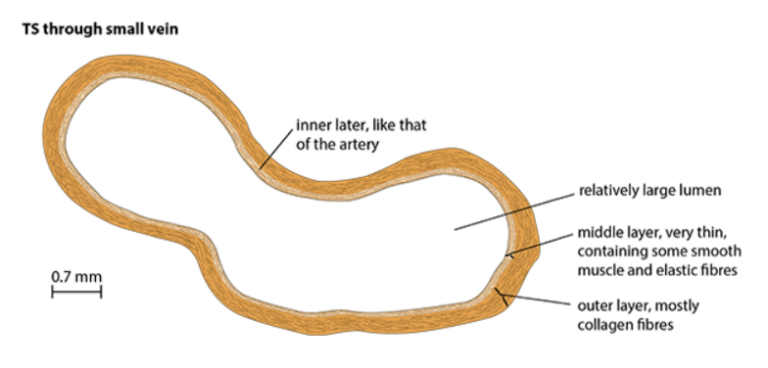
Veins and venules
- Capillaries join to form venules, which then merge into veins, responsible for returning blood to the heart
- Blood pressure in veins is very low (typically around 5 mmHg or less) so vein walls are thinner and have fewer elastic and muscle fibers than arteries
- Many veins (especially in the legs) are located near muscles
- Muscle contractions squeeze veins, temporarily raising pressure and assisting blood flow
- Semilunar valves in veins ensure blood flows only towards the heart by preventing backflow, enabling upward movement of blood when muscles contract
Blood pressure
- Blood pressure is highest when blood leaves the heart and gradually decreases as it moves through arteries, arterioles, capillaries, venules, and veins
- This pattern occurs in both the systemic and pulmonary systems
- Systemic blood pressure is higher than pulmonary blood pressure, reflecting the greater distance and resistance in the systemic circulation
8.3 Tissue fluid
- Blood plasma is mostly water, with dissolved nutrients, waste products, and plasma proteins
- Plasma leaks out of capillaries into tissue spaces, forming tissue fluid
- Tissue fluid is similar to blood plasma but contains fewer proteins and no red blood cells, though some white blood cells can move through it
- The movement of fluid from capillaries to tissue fluid is due to blood pressure at the arterial end, which is counteracted by the concentration of proteins in blood plasma (lower water potential) that pulls water back in (via osmosis)
- At the venule end of the capillary bed, blood pressure drops, and the water potential gradient causes fluid to move back into the capillaries
- Overall, more fluid exits capillaries than enters
- Resulting in a net loss of fluid from the blood
- Collected by lymphatic vessels
- High blood pressure can cause excessive fluid leakage, leading to edema
- Arterioles help reduce blood pressure before it enters the capillaries to prevent fluid buildup
- Tissue fluid is the environment for body cells, enabling exchanges of materials, and is crucial for homeostasis

8.4 Blood
- The body contains about 5 dm³ of blood, with a mass of approximately 5 kg
- Blood plasma is 95% water, with substances such as glucose, urea, and heat transported throughout the body
- Glucose is transported from the small intestine to the liver and then to other cells
- Urea is transported from the liver to the kidneys
- Blood plasma also transports heat due to water’s high heat capacity, which helps regulate the body’s temperature
- Water’s solvent properties make blood plasma effective in transporting these substances
- Tissue fluid, which is derived from blood plasma, also contains a high percentage of water, aiding in maintaining a constant body temperature
Red blood cells
- Red blood cells (RBCs) contain haemoglobin, which gives them their red color and allows oxygen transport from the lungs to tissues
Features
- Shape: biconcave disc increases surface area to volume ratio, facilitating quick oxygen diffusion
- Size: small (~7 μm in diameter), allowing efficient gas exchange and enabling RBCs to pass through narrow capillaries
- Flexibility: RBCs can be squashed due to a specialized cytoskeleton of protein fibers, enabling them to pass through narrow vessels and return to normal shape
- Lack of organelles: no nucleus, mitochondria, or endoplasmic reticulum, maximizing space for hemoglobin and oxygen-carrying capacity
- Lifespan: RBCs have a short lifespan, being broken down in the liver and constantly replaced in the bone marrow.
Haemoglobin
- The circulatory system’s major role is to transport oxygen from alveoli in the lungs to tissues throughout the body
- Body cells require a constant supply of oxygen for aerobic respiration
- Oxygen is carried in red blood cells by haemoglobin
- Each haemoglobin molecule consists of four polypeptides, each with one haem group
- Each haem group can bind to one oxygen molecule (O2)
- One haemoglobin molecule can carry four oxygen molecules or eight oxygen atoms
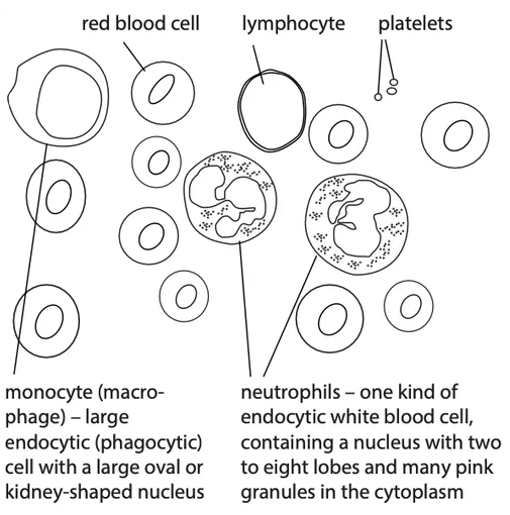
White blood cells
- White blood cells (WBCs) are produced in the bone marrow and are larger than red blood cells.
Features
- Have a nucleus (shape varies by type)
- Larger than RBCs, with lymphocytes being smaller than most other types
- Shape: spherical or irregular
- WBCs are divided into phagocytes and lymphocytes
- Phagocytes (e.g. neutrophils and monocytes) destroy microorganisms via phagocytosis
- Neutrophils have a lobed nucleus
- Monocytes can develop into macrophages
- Lymphocytes destroy microorganisms by secreting antibodies and have a large, round nucleus with minimal cytoplasm
- Phagocytes (e.g. neutrophils and monocytes) destroy microorganisms via phagocytosis
8.5 Transporting oxygen and carbon dioxide
The oxygen dissociation curve
- Haemoglobin’s function is to pick up oxygen in the lungs and release it to respiring tissues.
- Blood samples are exposed to different oxygen partial pressures, measuring percentage saturation (how much oxygen they combine with) ⇒ studying haemoglobin’s behaviour
- At low oxygen pressures, haemoglobin’s percentage saturation is low; at high pressures, it’s very high
- In the lungs, where oxygen pressure is high, haemoglobin is about 95-97% saturated with oxygen
- In actively respiring muscles, where the oxygen pressure is low, haemoglobin is only 20-25% saturated
- This allows haemoglobin to carry oxygen from the lungs to muscles, where it releases most of the oxygen for respiration.
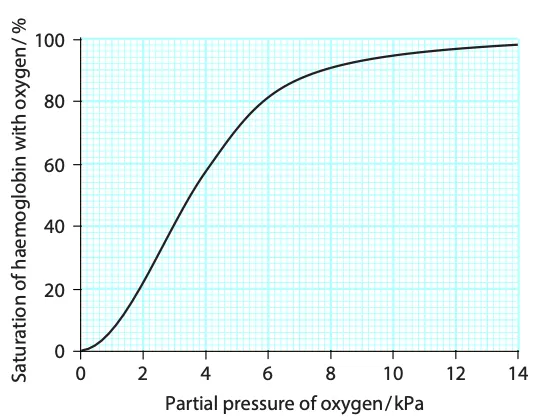
The S-shaped curve
- Haemoglobin’s shape changes when it combines with oxygen, making it easier for more oxygen molecules to bind
- Each haemoglobin molecule has four haem groups, each capable of binding to an oxygen molecule
- When the first oxygen molecule binds, the 3D structure of the haemoglobin changes, making it easier for the second, third, and fourth molecules to bind
- This explains the steep part of the haemoglobin dissociation curve, where a small change in oxygen partial pressure leads to a large change in the amount of oxygen bound to haemoglobin
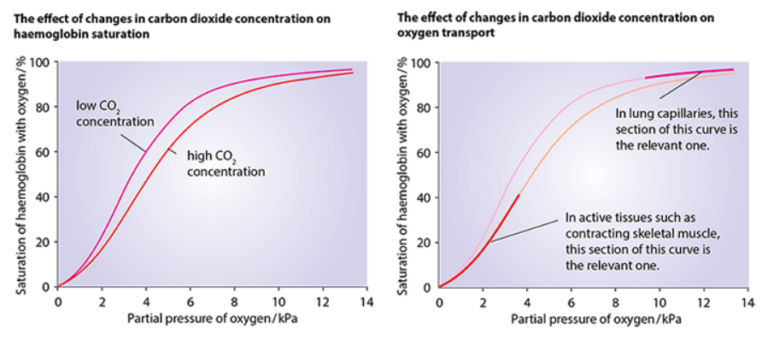
The Bohr shift
- Haemoglobin’s ability to pick up oxygen in the lungs and release it in tissues is enhanced by the presence of carbon dioxide
- Carbon dioxide diffuses into red blood cells, where it combines with water to form carbonic acid
\[
\text{CO}_2 + \text{H}_2\text{O} \xrightarrow{\text{Carbonic Anhydrase}} \text{H}_2\text{CO}_3
\]
- This reaction is catalysed by carbonic anhydrase in the cytoplasm of RBC
- The carbonic acid dissociates into hydrogen ions and hydrogen carbonate ions
\[
\text{H}_2\text{CO}_3 \leftrightarrow \text{H}^+ + \text{HCO}_3^-
\]
- Haemoglobin binds to the hydrogen ions, forming haemoglobin acid (HHb), which causes haemoglobin to release its bound oxygen
- The increased concentration of carbon dioxide in actively respiring tissues leads to a lower pH, promoting haemoglobin to release oxygen more readily
- Bohr Shift and the dissociation curve: when the carbon dioxide levels are high, the dissociation curve shifts to the right
- This means that at the same level of oxygen, haemoglobin holds less oxygen than it would at lower carbon dioxide levels
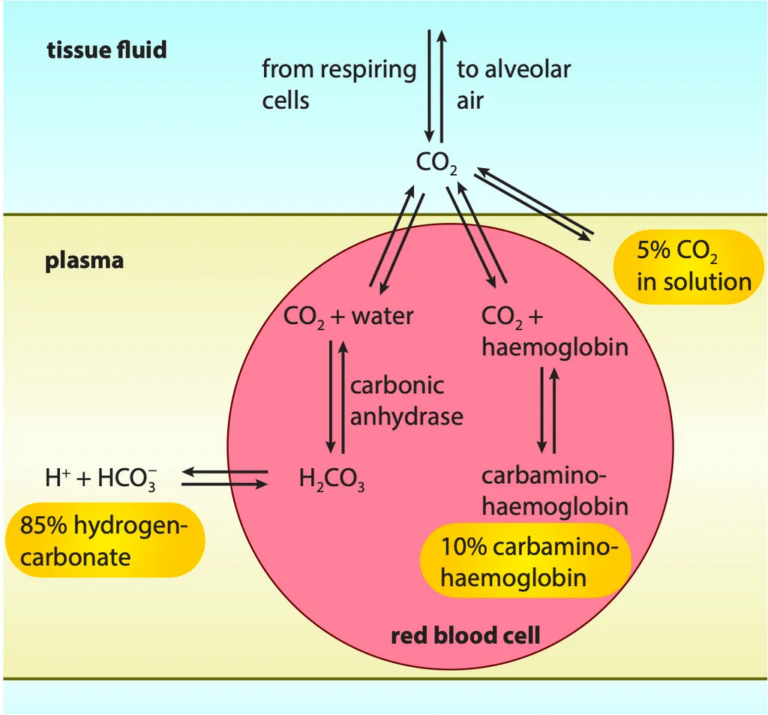
The chloride shift
- Hydrogen carbonate ions are produced inside red blood cells when carbonic anhydrase acts on carbon dioxide
- These ions diffuse out of the RBCs into the blood plasma
- To balance this, chloride ions (Cl–) move from the plasma into the red blood cells
- Without the chloride shift, the inside of the red blood cell would become positively charged because hydrogen ions would accumulate
- Chloride ions entering the cell help prevent it from becoming too positively charged since hydrogen ions can’t leave the cell due to the cell membrane’s impermeability
Carbon dioxide transport
- Carbon dioxide is produced by respiring cells throughout the body
- Blood carries carbon dioxide from the cells to the lungs
- In the lungs, carbon dioxide diffuses into the alveoli to be expelled from the body
- Carbon dioxide is transported in the blood in three different ways
As hydrogen carbonate ions in the blood plasma
- Dissolved carbon dioxide dissociates into hydrogen carbonate ions
- Hydrogen carbonate ions are formed in the cytoplasm of red blood cells, where carbonic anhydrase is found
- Most hydrogen carbonate ions diffuse out of red blood cells into the blood plasma
- Around 85% of the carbon dioxide transported by the blood is carried as hydrogen carbonate ions in solution
As dissolved carbon dioxide in the blood plasma
- Some carbon dioxide remains as carbon dioxide molecules
- A small portion of this carbon dioxide dissolves directly in the blood plasma
- About 5% of the total carbon dioxide in the blood is carried in this dissolved form
As carbaminohaemoglobin
- Some carbon dioxide molecules diffuse into red blood cells but do not react with carbonic anhydrase
- These molecules instead combine with terminal amine groups (–NH2) of some haemoglobin molecules, forming carbaminohaemoglobin
- About 10% of carbon dioxide is carried in this form
- When blood reaches the lungs, the carbon dioxide concentrations in the alveoli are lower than in the blood, causing carbon dioxide to diffuse from the blood into the alveoli
- This diffusion triggers the release of carbon dioxide from carbaminohaemoglobin in red blood cells
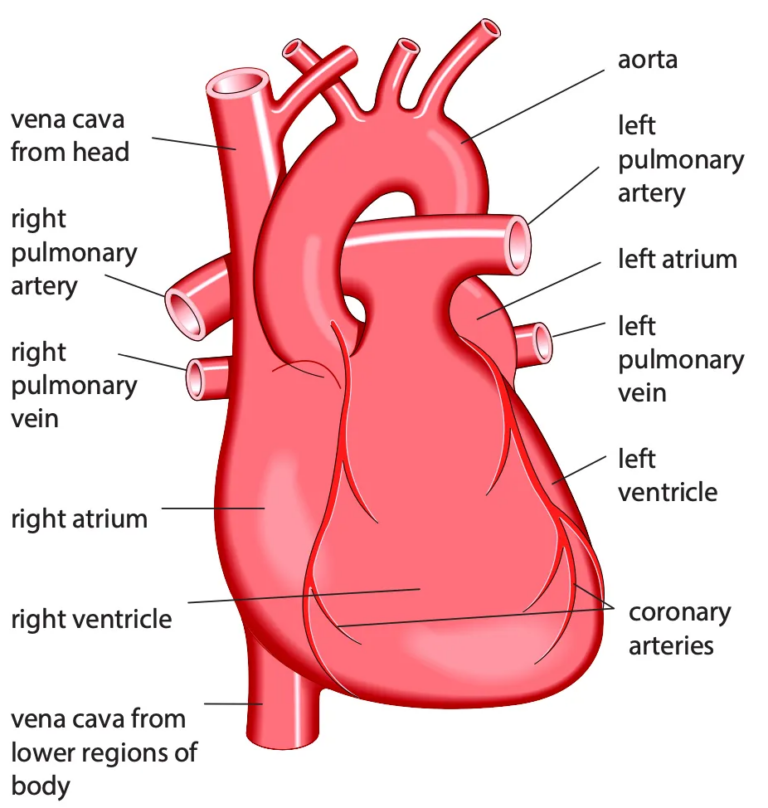
8.6 The heart
- The adult human heart has a mass of around 300g and is about the size of a fist
- The muscle of the heart is called cardiac muscle, made of interconnecting cells with tightly joined cell membranes
- The close contact between muscle cells allows electrical excitation to pass easily
- The coronary arteries, branching from the aorta, deliver oxygenated blood to the heart muscle
- The heart has four chambers: two atria and two ventricles, separated by the septum
- The atria receive blood from the veins
- The right atrium receives blood from the venae cavae
- The left atrium receives blood from the pulmonary veins
- The ventricles pump blood into the arteries
- The left ventricle pumps into the aorta
- The right ventricle pumps into the pulmonary arteries
- Atrioventricular valves separate the atria from the ventricles
- The left valve is the mitral or bicuspid valve
- The right valve is the tricuspid valve
- Semilunar valves separate the ventricles from the arteries
The cardiac cycle
✅ Cardiac cycle (definition)
The sequence of events that takes place during one heartbeat
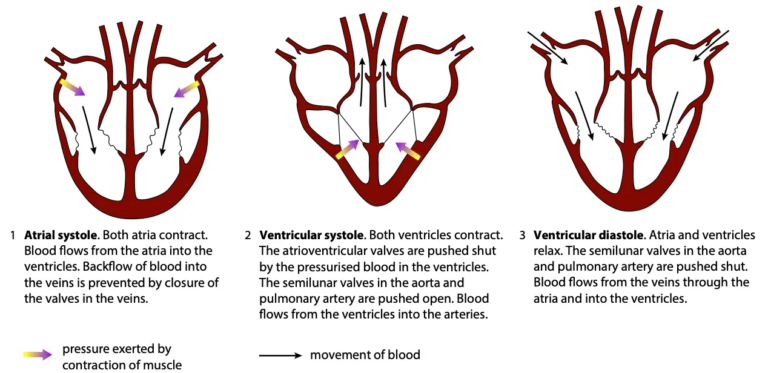
- The heart beats about 70 times per minute, with the cardiac cycle making up one heartbeat
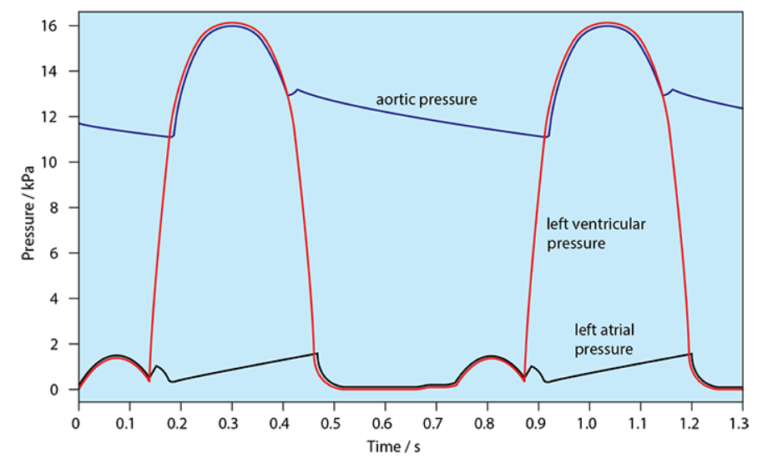
- The cycle begins when the heart is filled with blood, and the atrial walls contract (atrial systole)
- The pressure from this contraction is not very high, but it forces blood into the ventricles through the atrioventricular valves
- Backflow into the pulmonary veins and venae cavae is prevented by semilunar valves in these veins
- About 0.1 seconds after atrial systole, the ventricles contract (ventricular systole)
- The thick ventricular walls squeeze inward, increasing blood pressure and pushing blood out into the arteries
- As the pressure in the ventricles exceeds that in the atria, the atrioventricular valves close, preventing backflow into the atria
- Blood moves upwards into the aorta and pulmonary artery, opening the semilunar valves
- Ventricular systole lasts for about 0.3 seconds, after which the ventricles relax (ventricular diastole)
- Pressure drops in the ventricles, and the semilunar valves close, preventing blood from flowing back into the ventricles
- During ventricular diastole, blood flows into the atria from the veins, and some blood trickles into the ventricles through the atrioventricular valves
- The atrial muscle contracts, pushing blood into the ventricles, starting the cycle again
- Comparison of atrial and ventricular walls
- The ventricles have much thicker walls than the atria, as they need to generate more force to pump blood around the body
- Comparison of the walls of the right and left ventricles
- The right ventricle pumps blood to the lungs, requiring less force since the lungs are close to the heart, and high pressure could damage lung capillaries
- The left ventricle pumps blood to the rest of the body, requiring more force, with thicker muscle walls compared to the right ventricle
- Arterioles help reduce pressure before blood enters capillaries, but during exercise, arterioles supplying muscles dilate to increase blood flow
- The left ventricle must still generate enough pressure to supply blood to other organs during exercise
Control of the heartbeat
- Cardiac muscle is myogenic, meaning it can contract and relax naturally without nerve impulses
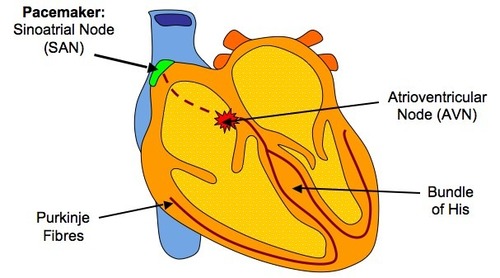
- The heart has its own built-in controlling system to ensure coordinated contractions, initiated by the sinoatrial node (SAN), also known as the pacemaker
- The SAN sets the rhythm for all other cardiac muscle cells, causing the atrial walls to contract almost simultaneously
- The ventricles contract slightly later than the atria to prevent simultaneous contractions
- A band of non-conductive fibers between the atria and ventricles temporarily delays the electrical signal as it moves from the atria to the ventricles
- The signal is transmitted through the atrioventricular node (AVN) after a brief delay of about 0.1 seconds
- The AVN passes the signal to the Purkyne tissue, which transmits it rapidly through the septum to the ventricles
- This causes the ventricles to contract from the bottom upwards, pushing blood into the arteries