AS Level Biology 9700
10. Infectious diseases
Written by: Rhia Sakthivel
Formatted by: Pranav I
Index
10.1 Infectious diseases
✅ Disease (definition)
- Abnormal condition (1 mark)
- Any of the below (1 mark)
- Having an adverse effect on an organism
- Reduces the effectiveness of functions
- Produces specific symptoms
- Infectious and non-infectious diseases
✅ Infectious disease (definition)
- A disease caused by a pathogen (1 mark)
- Can be passed from one organism to another (1 mark)
- Causes ill health (1 mark)
Cholera
- Pathogen: Vibrio cholerae (bacteria)
- Site of action: gut (small intestine)
- Toxins prevent the intestine wall from absorbing water
Transmission
- An infected person passes out faeces containing V. cholerae
- Faeces contaminate water sources and crops
- An uninfected person ingests contaminated water or food
Symptoms
- Diarrhea (watery faeces)
- This leads to dehydration → the loss of water and salts from the body
- Could be lethal without treatment
Treatment
- Fluid and salt replacement via oral rehydration therapy or intravenous therapy (IV fluids)
- Antibiotics
Prevention
- Set up proper sewage treatment plant & water treatment plant
- Boil/treat water before drinking to kill bacteria
- Practice proper sanitation by washing hands with soap after going to the toilet & before handling food
- Cook food using clean cooking utensils
- Avoid using human faeces as fertilizers
- Encourage vaccination
- Oral vaccines for temporary protection against cholera (especially before traveling to a region with a cholera outbreak)
- Rapid diagnosis and rapid treatment using ORS to reduce the spread of cholera to other people
- Mandatory quarantine for cholera-infected patients
Biological, social and economic factors (common questions)
- What factors cause outbreaks in a country?
- Poor personal hygiene (not washing hands with soap after using the toilet)
- Natural disasters such as tsunamis and earthquakes
- Do not have proper sewage treatment plant & water treatment plant
- Water sources and crops contaminated with sewage.
- Low level of awareness about the prevention of cholera
- Lack of availability of cholera vaccines & antibiotics
- Collapse of health system, lack of trained professionals
- Slow diagnosis
- Why are outbreaks common after natural disasters?
- Poor sanitation
- Disruption to healthcare facilities
- Damage to sewers/drains/water systems
- Mixing of sewage and drinking water
- Water supplies cannot be treated
Malaria
- Pathogens: all are protoctists
- Plasmodium falciparum
- Plasmodium malariae
- Plasmodium ovale
- Plasmodium vivax
- Site of action: red blood cells, liver and brain
Transmission
- Female Anopheles mosquito is the vector
- When the mosquito bites an infected person, the parasite enters its body
- The mosquito bites an uninfected person and secretes an anticoagulant (blood clot prevention chemical)
- The parasite enters the blood of the uninflected person during the blood meal
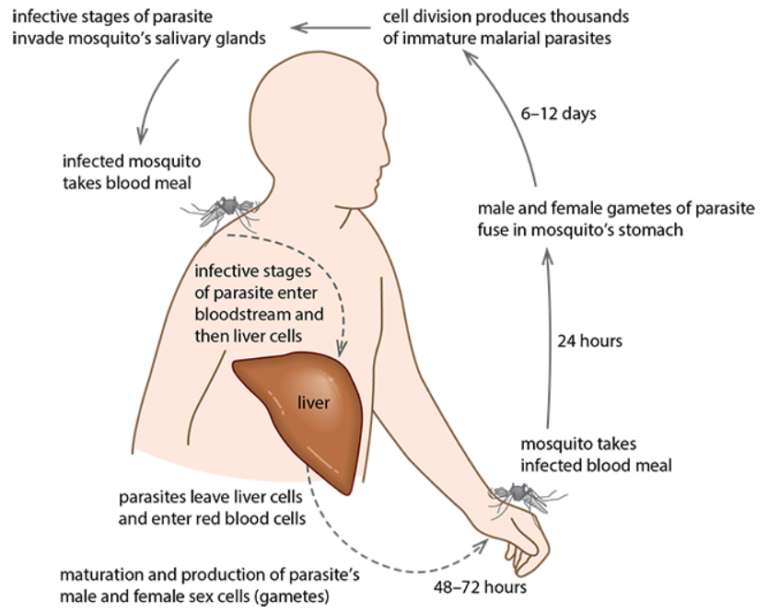
Plasmodium life cycle
- Female Anopheles mosquito feeds on human blood
- If the person it bit is infected, it will take some of the pathogen’s gametes with the blood meal
- Male and female gametes fuse in the mosquito’s gut which form infective stages and move to the salivary gland
- When the mosquitos feed again, the infective stages pass from the mosquito’s salivary glands into the human blood along with an anticoagulant
- Parasites enter red blood cells where they multiply and spread
Symptoms
- Fever
- Anaemia
- Headaches
- Nausea
- Shivering
Treatment
- Cases to be confirmed through a test
- Anti-malarial drugs:
- Quinine & chloroquine for infected people
- Proguanil as a preventative
- Mefloquine is a newer drug
- Drug resistance is becoming widespread
- Most efficient treatment: artemisinin-based combination therapy (ACT) where drugs derived from the Artemisia annua plant are used in combination with other drugs (such as mefloquine)
- Prophylactic drugs are taken before, during, and after visiting an area where malaria is endemic
Prevention
- Controlling malaria:
- Reduce the number of mosquitos
- Avoid being bitten by mosquitos
- Use prophylactic drugs to prevent infection
- Sleep in mosquito nets treated with long-lasting insecticides
- Use mosquito repellents
- Stocking ponds, irrigation, and permanent bodies of water with fish that feeds on mosquito larvae
- Spray a preparation containing Bacillus thuringiensis which kills mosquito larvae without harming other organisms
- Spread oil on small water surfaces to disallow the breathing of larvae
- Pregnant women and young children are treated with prophylactic drugs
- Encourage vaccination among young children. (Mosquirix → provides partial protection against malaria)
- Rapid testing (dipstick test)
Tuberculosis (TB)
- Pathogens: both are bacteria
- Mycobacterium tuberculosis
- Mycobacterium bovis
- Site of action:
- Primary infection → lungs
- Secondary infection → lymph nodes, bones, and gut
Transmission
- An infected person coughs, sneezes, or breathes out
- Droplets contain pathogen
- Droplets in the air are inhaled by the uninfected person
- Consumption of milk and/or meat containing the pathogen (this is for M. bovis, which occurs in cattle)
Symptoms
- An infected person coughs, sneezes, or breathes out
- Droplets contain pathogen
- Droplets in the air are inhaled by the uninfected person
- Consumption of milk and/or meat containing the pathogen (this is for M. bovis, which occurs in cattle)
Treatment
- Diagnosis:
- Sample of sputum (mucus & pus) collected from lungs for testing
- Identification of the pathogen can be done quickly via microscopy
- Treatment:
- People are isolated at the most infectious stage
- Several antibiotics to ensure bacteria are killed (if not killed, drug resistance can form)
- Treatment is long → 6-9 months (some people do not finish the course of treatment thinking they are cured, leading to drug resistance)
- Drugs used: isoniazid and rifampicin
Prevention
- The government provides proper housing to poor, homeless people
- Avoids overcrowded living conditions that increase the risk of transmission
- Cattle are regularly tested for TB
- Pasteurize milk
- Cook meat properly
- To prevent TB infection caused by M. bovis
- Encourage vaccination of BCG vaccines
- Contact tracing, rapid diagnosis, and rapid treatment to reduce the spread of TB
- Mandatory quarantine for TB patients, especially during the most contagious period (two to four weeks)
- Health workers/family members must ensure TB patients complete their course of treatment
- To prevent harboring strains of TB bacteria that are antibiotic resistant
Biological, social and economic factors (common questions)
- Discuss factors influencing the increase in TB cases
- Overcrowded and poorly ventilated living environments
- Failure in vaccination programs (herd immunity not achieved)
- TB patients do not complete the course of antibiotics, increasing the risk of bacteria undergoing mutations, thus developing antibiotic resistance
- Increase in number of HIV cases → TB is an opportunistic infection
- Latent TB becomes active.
- Diagnosis is difficult when the pathogen remains dormant
- Limited education and awareness about TB
HIV/AIDS
- Pathogen: human immunodeficiency virus (HIV)
- Infection with HIV may lead to acquired immunodeficiency syndrome (AIDS)
- HIV is a retrovirus (RNA genetic material)
- Site of action: T-helper lymphocytes and macrophages
Transmission
- Via direct exchange of bodily fluids such as
- Semen and vaginal fluids during sexual intercourse
- Blood transfusions
- Sharing of needles by intravenous drug users
- Mother to fetus across the placenta, and mixing of blood during birth
- Mother to infant via breastmilk
Symptoms
- HIV: flu-like symptoms and then becomes symptomless
- AIDS: opportunistic infections including TB, pneumonia, cancers, diarrhea, fever, sweating, weight loss, and dementia
Treatment
- There is no cure for AIDS and no vaccine for HIV
- Drug therapy can slow down the onset of AIDS so that infected people can lead normal lives
- Drugs are expensive
- Have side effects
- Combination therapy can be hard to follow because there are strict timings to take drugs and if not followed, drug resistance can develop
Prevention
- Difficult due to the long latent stage
- Use condoms, femidoms, or dental dams during sexual intercourse to avoid direct contact with body fluids.
- Blood collected from donors is screened for HIV
- Blood is heat-treated to kill any virus present
- Intravenous drug users are advised to give up their habit or prevent sharing hypodermis syringes
- Needle exchange schemes are operated at some places to exchange used needles with sterile ones
- Contact tracing: when infected people identify those they might have infected so that they can be tested early on
- Infected mothers are treated with antiretroviral drugs to reduce the risk of infants being infected with HIV
- Infected mothers are advised not to breastfeed their babies
- Public awareness: people should know about HIV and how to protect themselves
10.2 Antibiotics
✅ Antibiotics (definition)
A drug derived from living organisms that kills (or stops the growth of bacteria) without harming the cells of the infected organism
How they work
- They inhibit factors of growth/metabolism in bacteria, including:
- Synthesis of peptidoglycan cell wall
- Protein activity in the cell membrane
- Enzyme action
- DNA synthesis
- Protein synthesis
Why do antibiotics not work on viruses
- Viruses are NOT living organisms
- Antibiotics cannot act on the capsid of viruses
- Viruses do not possess cellular structures such as cell walls
- Antibiotics may not be able to reach viruses inside the host cell
How does penicillin work?
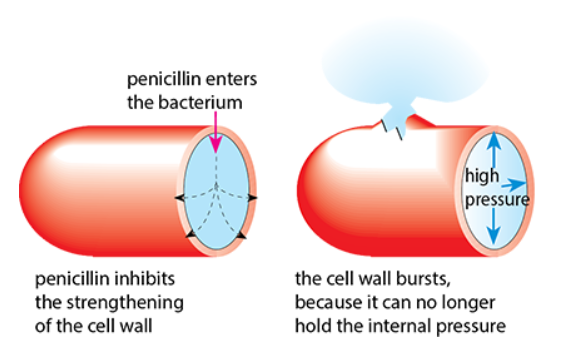
- Penicillin targets the peptidoglycan cell wall of bacteria
- Preventing the formation of cross-links between peptidoglycan chains
- It inhibits the action of transpeptidase which forms the cross-links
- Autolysins continue to make small holes in the cell wall, but no crosslinks are formed to fill the gaps
- This weakens the cell wall, making it unable to withstand high turgor pressure
- When endosmosis occurs, the bacterium bursts
🚨 Only acts on growing bacteria
Antibiotic resistance
✅ Antibiotic resistance (definition)
The ability of bacteria to grow in the presence of antibiotics that would typically slow their growth/kill them
- Arises due to mutation
- Becomes widespread when antibiotics are overused
Consequences of antibiotic resistance
- Patients may have to stay in hospitals longer, where they can develop severe conditions
- This can lead to infecting more uninfected people
- There is a constant race to find new antibiotics as resistant strains keep arising
How resistance spreads
- Misuse of antibiotics (such as taking them for viral infection)
- When patients do not complete the course of antibiotics
- Antibiotics cause selective pressure
- Natural selection takes place → susceptible bacteria are killed whereas bacteria with resistance survive
- Reproduce and pass on the gene for resistance to offspring
- Vertical transmission (asexual reproduction through binary fission)
- Horizontal transmission (transferring of plasmid during conjugation)
- Thus, the frequency of resistance increases in the bacterial population
Reducing its impact
- Antibiotics should be chosen carefully
- Make more semi-synthetic antibiotics (slightly chemically altered) to extend the range of available antibiotics
Preventing resistance
- Use antibiotics only when necessary
- Reduce the number of countries where antibiotics are sold without a prescription
- Avoiding the use of wide-spectrum antibiotics; use narrow-spectrum antibiotics
- Complete the full course of medication
- Do not keep unused antibiotics for self-medication or other people
- Change the type of antibiotics prescribed for certain diseases so that the same antibiotic is not prescribed for the same diseases
- Avoid using antibiotics in farming
- Soil bacteria can gain and spread resistance